INTRODUCTION
ST-segment elevation myocardial infarction (STEMI) is a severe form of heart attack characterized by a prolonged period of blocked blood supply that affects a large area of the heart muscle 1. The mean age of a first MI is 65.1 for men, while for women, it is 72. An ST-elevation myocardial infarction affects around 38% of patients with acute coronary syndrome when they arrive at the hospital 2.
STEMI is commonly caused by the rupture of an atherosclerotic plaque in a coronary artery, leading to the formation of a blood clot that completely blocks the artery and interrupts blood flow to the heart muscle. This results in myocardial ischemia and, if not promptly treated, irreversible damage to the heart muscle 1,2.
The symptoms of STEMI can include chest pain or discomfort, shortness of breath, nausea, lightheadedness, and pain or discomfort in other areas of the upper body, such as the arms, back, neck, jaw, or stomach 3.
Diagnosis of STEMI is primarily based on the clinical presentation, ECG findings, and the elevation of cardiac biomarkers. An ECG demonstrating ST-segment elevation is considered diagnostic, particularly when complemented by symptoms indicative of ischemia. Furthermore, cardiac enzymes such as troponins are utilized to confirm myocardial damage 1,4.
Treatment of STEMI focuses on the timely restoration of coronary blood flow, typically achieved through reperfusion therapies such as percutaneous coronary intervention (PCI) or thrombolytic therapy 5. Adjuvant therapies include antiplatelet agents, anticoagulants, beta-blockers, and angiotensin-converting enzyme inhibitors to reduce myocardial oxygen demand and prevent further thrombus formation 6,7.
In this context, recombinant human brain natriuretic peptide (rhBNP) therapy emerges as a novel adjunct in managing STEMI. rhBNP, a synthetic form of the naturally occurring brain natriuretic peptide, has shown promise in improving ventricular function and hemodynamics 8. Its mechanisms of action include vasodilation, natriuresis, and the inhibition of the renin-angiotensin-aldosterone system, which collectively contribute to reduced cardiac load and improved myocardial recovery 9. According to a study by Zhou et al.10, rhBNP has shown promise in improving ventricular function and hemodynamics in patients with end-stage renal disease and type 4 cardiorenal syndrome. Another study by Liang et al. suggests that rhBNP combined with catheter-directed therapy may improve right ventricular dysfunction and stabilize hemodynamics in patients with acute pulmonary embolism 11.
Given the high stakes of STEMI management and the potential impact on patient outcomes, a comprehensive evaluation of rhBNP’s efficacy and safety is warranted. Since limited studies have been conducted in this field, especially in the Middle East, this study was essential to elucidate the effect of the therapeutic effect of recombinant human brain natriuretic peptide in patients with myocardial infarction by increasing the ST piece.
MATERIALS AND METHODS
General information
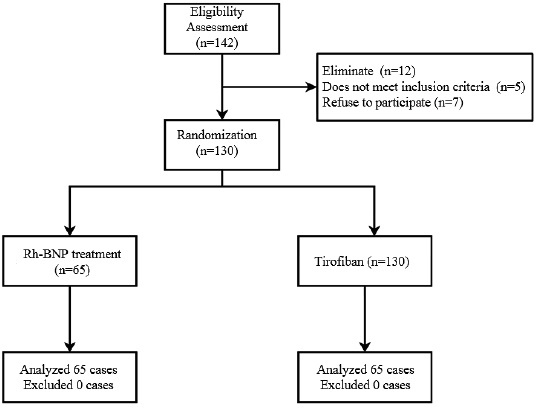
The research is a retrospective study using case data. The criteria for selecting patients in this study were as follows: the diagnosis of STEMI symptoms following views of the “STEMI Diagnosis and Treatment Guidelines” 6; patients received PCI treatment within 12 h after admission; treatment with tirofiban (TIF) or rh-BNP after PCI; no allergic reactions were observed after treatment with TIF or rh-BNP; did not receive intravenous thrombolysis treatment before PCI; Killip level exceeds that of Grade III or cardiogenic shock patients. Exclusion criteria: patients with comorbidities of organ and tissue diseases such as brain, heart, kidney, and liver; patients with severe aortic stenosis; patients with mental or other cognitive impairments or who refuse to cooperate with the experiment; patients with pulmonary hypertension caused by pulmonary heart disease or other reasons; patients with a history of MI, valvular heart disease, dilated cardiomyopathy, HF, hypertrophic cardiomyopathy, or other general diseases. Given the above standards, this study collected the medical history information of 142 STEMI patients admitted to our hospital from June 2021 to June 2023, with 130 participants included in the experimental study. In the queue, 65 patients received treatments with TIF, while the remaining cases received treatments with rh-BNP. All sufferers had clinical and pathological features taken and signed an informed consent form to use this information. This research was approved by the Ethics Committee of the Medical Center to collect relevant information from sufferers (approval number: MEC-2021-06). All work was carried out following the provisions of the Declaration of Helsinki. The research process is demonstrated in Fig. 1.
Treatment strategies
All patients took 300 mg aspirin orally, clopidogrel 300 mg/ticagrelor 180 mg, and intravenous heparin 5000 IU at admission. Coronary artery angiography (CAG) was carried out before intervention to determine the quantity of the pathological branches, for patients who received treatments with rh-BNP, 5 mg of medication was injected intravascularly during the intervention period, followed by implantation of a stent and re-administration of 5 mg of rh-BNP. If the symptoms of slow BF persisted, they were given a last 5 mg dose of rh-BNP. Sufferers who received treatments with TIF were slowly injected 5 mg/kg through the CA during the intervention period. After the stent implantation, 5 mg/kg TIF was administered via CA again. 3 mg/kg TIF was injected through the CA for sufferers with slow BF symptoms. After 24 hours of intervention, all patients were given aspirin 100 mg, clopidogrel 75 mg/ticagrelor 90 mg and heparin 5000 IU for 5-7 days. Patients were followed up for 30 days after discharge, and MACE (Major Adverse Cardiovascular Events) were recorded.
Measurement of treating outcomes
The myocardial infarction thrombolysis (TMI) classification, hemodynamic parameters, thrombotic score (TS) 7, left ventricular ejection fraction (LVEF), CRP level, uric acid, liver and kidney functions, electrocardiogram (ECG), echocardiography and other information of patients before and after the intervention were collected to compare differences in the therapeutic effects (treatment efficacy) and SE of the two treatment methods.
Statistical analysis
Relevant analysis was conducted using the SPSS version 19.0 software (IBM®, Armonk, NY). Continuous data was denoted by mean ± standard deviation (SD). The number of cases denotes classified data. The Student test was used to compare the differences between consecutive data sets. Chi-square and Fisher’s exact tests were used to determine whether there are differences between different categories of index groups. p<0.05 is statistically significant.
RESULTS
Patient baseline characteristics
The analysis of baseline data among the sufferers participating in this experiment did not demonstrate significant differences (SD) in preoperative age, body mass index (BMI), and other indicators. Table 1 demonstrates the details.
Table 1 Baseline Characteristics.
| Characteristic | rh-BNP(n=65) | TIF(n=65) | t/χ2 | p |
|---|---|---|---|---|
| Age (years) | 60.19±10.02 | 58.96±10.14 | 1.462 | 0.09 |
| Gender (male, %) | 47(72.3) | 51(78.5) | -0.613 | 0.36 |
| BMI(kg/m2) | 25.94±3.54 | 25.44±3.29 | 0.837 | 0.50 |
| Time before balloon dilation(min) | 227.98±68.52 | 232.19±86.43 | -0.388 | 0.63 |
| Killip classification | ||||
| Level 1 (n, %) | 61(93.8) | 60(92.3) | 0.117 | 0.69 |
| Level 2 (n, %) | 4(6.2) | 5(7.7) | ||
| Smoke (n,%) | 41(63.1) | 40(61.5) | 0.035 | 0.85 |
| Drink (n,%) | 24(36.9) | 14(21.5) | 3.710 | 0.06 |
| Hypertension (n, %) | 41(63.1) | 47(72.3) | 1.258 | 0.27 |
| Level 1 (n, %) | 8(12.3) | 7(10.8) | ||
| Level 2 (n, %) | 16(24.6) | 14(21.5) | 0.286 | 0.85 |
| Level 3 (n, %) | 17(26.2) | 19(29.2) | ||
| Diabetes (n, %) | 18(27.7) | 21(32.3) | 0.328 | 0.56 |
| Cerebral Infarction (n, %) | 8(12.3) | 11(16.9) | 0.525 | 0.49 |
t: t-test; χ2: Chi-squared test; BMI: body mass index; rh-BNP: B-type recombinant human brain peptide. TIF: tirofiban.
No statistically significant differences were among the sufferers participating in this experiment in combined medication (Table 2).
Table 2 Information on drug combination use.
| Characteristic | rh-BNP (n=65) | TIF (n=65) | t/χ2 | p value |
|---|---|---|---|---|
| Ticagrelor (n, %) | 59(90.8) | 61(93.8) | - | 0.39 |
| Statins (n, %) | 62(95.4) | 61(93.8) | - | 0.53 |
| Nitrates (n, %) | 45(69.2) | 48(73.8) | 0.443 | 0.44 |
| β-blocker (n, %) | 57(87.7) | 52(80.0) | 1.690 | 0.13 |
| ACEI/ARB | 52(80.0) | 56(86.2) | 1.259 | 0.29 |
| CCB (n, %) | 21(32.3) | 22(33.8) | 0.884 | 0.36 |
| PPI (n, %) | 48(73.8) | 52(80.0) | 0.705 | 0.44 |
| Hypoglycemic drugs (n, %) | 21(32.3) | 23(35.4) | 0.327 | 0.53 |
t: t-test, χ2: Chi-squared test; rh-BNP: B-type recombinant human brain natriuretic peptide; TIF: tirofiban; ACEI: ACE inhibitor; ARB: angiotensin II receptor antagonist; CCB: calcium channel blocker (calcium antagonist); PPI: proton pump inhibitor.
Intervention Information
Table 3 indicates no differences in the number of branches, number of stents, and score of thrombus before the intervention, systolic blood pressure, and other relevant respects. However, after the intervention, the TMI changes in thrombus score levels in the rh-BNP group and other relevant aspects dramatically exceeded those in the TIF group (Table 3). On the other hand, the TMI Frame Count (CTFC), slow flow (SF) incidence, post-intervention thrombus score, stent length, and sodium nitroprusside administration times after correction were dramatically ´lower in the TIFgroup (Table 3).
Table 3 Information on treatment outcomes for patients with myocardial infarction with elevation of the segment ST (STEMI) and percutaneous coronary intervention (PCI) patients.
| Characteristic | rh-BNP (n=65) | TIF (n=65) | t/χ2 | p value |
|---|---|---|---|---|
| Number of branches | ||||
| Single branch (n,%) | 8(12.3) | 7(10.8) | ||
| Double branches (n,%) | 19(29.2) | 17(26.2) | ||
| Three branches (n,%) | 38(58.5) | 41(63.1) | 0.286 | 0.87 |
| IRA distribution | ||||
| LAD (n,%) | 33 (50.8) | 38(58.5) | ||
| LCX (n,%) | 10 (15.4) | 7(10.8) | ||
| RCA (n,%) | 22 (33.8) | 20(30.8) | 0.977 | 0.61 |
| TMI level before PCI | ||||
| Level 0 (n,%) | 19(29.2) | 25(38.5) | 2.298 | 0.51 |
| Level 1 (n,%) | 8(12.3) | 8(12.3) | ||
| Level 2 (n,%) | 9(13.8) | 11(16.9) | ||
| Level 3 (n,%) | 29(44.6) | 21(32.3) | ||
| TMI level after PCI | ||||
| Level 0 (n,%) | 1(1.5) | 2(2.3) | - | 0.03 |
| Level 1 (n,%) | 2(3.1) | 7(6.9) | ||
| Level 2 (n,%) | 6(9.2) | 11(13.1) | ||
| Level 3 (n,%) | 56(86.2) | 45(77.7) | ||
| CTFC after PCI (FPS) | 23.60±4.05 | 25.57±5.29 | -2.381 | 0.02 |
| Level 3 TMPG after PCI (n,%) | 58(89.2) | 49(75.5) | 4.279 | 0.04 |
| TS score before PCI | 3(2,4) | 3(2,4) | -1.45 | 0.15 |
| TS score after PCI | 0(0,1) | 1(0,1) | -3.908 | <0.001 |
| TS score changes | 3(2,3) | 1(1,1) | -4.263 | <0.001 |
| Support number | 1(1,1) | 1(1,2) | -0.898 | 0.37 |
| Support length(mm) | 26.4±11.33 | 31.35±12.93 | -2.323 | 0.02 |
| Thrombotic aspiration during intervention (n,%) | 15(23.1) | 14(21.5) | 0.044 | 0.83 |
| Intraoperative hypotension (n,%) | 5(7.7) | 7(10.8) | 0.367 | 0.55 |
| Intraoperative systolic blood pressure (mmHg) | 125.58±18.87 | 122.88±21.06 | 0.772 | 0.44 |
| Intraoperative diastolic blood pressure (mmHg) | 70.66±5.09 | 70.69±11.50 | -0.2 | 0.98 |
| HR (n/min) | 72.23±8.46 | 72.58±7.65 | -0.25 | 0.80 |
| SF/no flow (n,%) | 9(13.8) | 20(30.8) | 5.370 | 0.02 |
| Use of sodium nitroprusside (n,%) | 4(6.2) | 15(23.1) | - | 0.01 |
t: t-test, χ2: Chi-squared test; rh-BNP: B-type recombinant human brain natriuretic peptide; TIF: tirofiban; CTFC: corrected TMI frame count; FPS: frames per second; IRA: infarction-related artery; LAD: anterior descending branch of left CA; LCX: left circumflex branch; PCI: primary PCI; RCA: right CA; rh-BNP: B-type recombinant human brain natriuretic peptide; TMI: thrombolysis for MI; TMPG: TMI myocardial perfusion level; TS: thrombotic score; HR: heart rate; SF: slow flow.
The effect of rh-BNP or TIF on the treating outcomes of PCI
Twenty-four hours after PCI intervention, creatine kinase (CK), creatine kinase isozyme (CKMB), and the amino-terminal fraction of B-type natriuretic peptide (NT pro-BNP) in the rh BNP group were dramatically lower than in the TIF group. The LEVF changes in the rh-BNP group (RBG) dramatically exceeded those in the TIF group. (Table 4).
Table 4 Effects of two treating methods on ventricular function and ejection fraction.
| Characteristic | rh-BNP (n=65) | TIF (n=65) | t/χ2 | p |
|---|---|---|---|---|
| CK peak (U/L) | 2108±1452 | 3562±1609 | 0.260 | 0.13 |
| CKMB peak (U/L) | 168.4±112.3 | 206.9±139.2 | 0.117 | 0.18 |
| Ln (NT-proBNP) | 5.96±0.75 | 7.43±0.93 | 0.122 | 0.15 |
| LEVF | 48.32±9.86 | 52.08±10.04 | 0.103 | 0.42 |
t: t-test, χ2: Chi-squared test; rh-BNP: B-type recombinant human brain natriuretic peptide; TIF: tirofiban; CK: creatine kinase; CKMB: creatine kinase isozyme; NT-proBNP: N-terminal pro B-type natriuretic peptide.
However, there were no statistical differences among the sufferers participating in this experiment in CK (p=0.13) and CKMB (p=0.18) at the peak recording time points. The sum STR in the RBG also markedly exceeded that in the TIF group immediately after intervention (Table 5), and there were no differences in sum STR two hours after the intervention (Table 5).
Table 5 The impact of two treatment methods on the total STR at two hours after PCI surgery.
| Characteristic | rh-BNP (n=65) | TIF (n=65) | t/χ2 | p |
|---|---|---|---|---|
| Total STR after PCI surgery | ||||
| <30% (n,%) | 5(7.7) | 12(18.5) | ||
| 30%-70% (n,%) | 13(21.5) | 21(32.3) | ||
| >70% (n,%) | 47(70.8) | 32(49.2) | 6.795 | 0.03 |
| Total STR at two hours after PCI surgery | ||||
| <30% (n,%) | 3(4.6) | 8(12.3) | ||
| 30%-70% (n,%) | 9(13.8) | 12(18.5) | ||
| >70% (n,%) | 53(81.5) | 45(69.2) | 3.408 | 0.17 |
t: t-test, χ2: Chi-squared test; Rh BNP: B-type recombinant human brain natriuretic peptide; TIF: tirofiban; PCI: primary PCI; STR: ST-segment resolution
Major Adverse Cardiovascular Events (MACE)
The incidence of angina and HF in the RBG was dramatically lower than in the TIF group (Table 6). On the other hand, in terms of CA occlusion microbleeds, the incidence of TMI microbleeds, the overall utilization of streptokinase, tissue type plasmin activator, and other relevant aspects in the RBG markedly exceeded those in the TIF group (Table 6). Both groups of patients did not experience MI or other severe side effects (Table 6).
Table 6 The impact of two treatment methods on the total STR at two hours after PCI surgery.
| Characteristic | rh-BNP (n=65) | TIF (n=65) | t/χ2 | p |
|---|---|---|---|---|
| Heart failure (n, %) | 11(16.9) | 23(35.4) | 5.735 | 0.03 |
| Mortality (n, %) | 1(1.5) | 0(0) | - | 0.32 |
| Angina pectoris (n, %) | 8(12.3) | 18(27.7) | 4.808 | 0.03 |
| TMI level | ||||
| Microbleeds (n, %) | 17(26.2) | 8(12.3) | 4.011 | 0.04 |
| GUSTO | ||||
| pyorrhea (n, %) | 17(26.2) | 8(12.3) | 4.011 | 0.05 |
t: t-test, χ2: Chi-squared test; PCI: primary PCI; STR: ST-segment resolution: rh-BNP: B-type recombinant human brain natriuretic peptide; TIF: tirofiban; TMI: thrombolysis myocardial infarction; GUSTO: the application of streptokinase and tissue type plasmin activator in the treatment of coronary occlusion.
Discharge follow-up
After discharge, there was no follow-up loss for 30 days. According to the information shown in Table 7, there were no differences in physiological indicators and MACE among the patients participating in this experiment (Table 7).
Table 7 The impact of two treatment methods on the total STR at two hours after PCI surgery.
| Characteristic | rh-BNP (n=65) | TIF (n=65) | t/χ2 | p |
|---|---|---|---|---|
| CK (U/L) | 82.50±27.29 | 80.66±29.18 | 0.369 | 0.71 |
| CKMB (U/L) | 12.58±6.76 | 12.63±6.91 | 0.046 | 0.95 |
| HSCRP (mg/L) | 2.18±1.09 | 2.52±1.61 | 1.381 | 0.16 |
| Ln (NT-proBNP) | 5.23±0.85 | 5.41±1.22 | 0.941 | 0.34 |
| LVEF (%) | 17(26.2) | 8 (12.3) | 4.011 | 0.04 |
| Mortality | 0 | 0 | - | - |
| Secondary MI | 0 | 0 | - | - |
| Treatment Failure | 5(7.8) | 9(13.8) | 1.209 | 0.26 |
| Angina pectoris | 7(10.9) | 5(9.3) | 0.427 | 0.55 |
t: t-test, χ2: Chi-squared test; PCI: primary PCI; STR: ST-segment resolution. rh-BNP: B-type recombinant human brain natriuretic peptide; TIF: tirofiban; CK: creatine kinase; CK-MB: creatine kinase-myocardial band; NT-proBNP: N-terminal pro b-type natriuretic peptide; LVEF: left ventricular ejection fraction.
DISCUSSION
PCI can markedly unblock the infarcted CA and was chosen as the first-line treatment strategy for STEMI clinical treatment. Recent studies given a large sample suggest that PCI can construct BF in >90% of IRA and restore TMI to level 3 12. However, the effect of PCI is offset by some severe side effects. Slow/no BF is a risk element influencing the prognosis of SEMI patients. Some drugs were utilized to enhance the therapeutic effect of PCI to enhance coronary BF after PCI.
Compared to studies with TIF, few people have focused on the influence of rh-BNP on coronary BF after PCI. Guo et al. showed that compared to patients treated with PCI alone, rh-BNP can significantly reduce the incidence of slow BF, indicating the potential of rh-BNP to improve BF after PCI 13. Therefore, this study compared the therapeutic influences of rh-BNP and TIF on PCI-related slow/no flow. The outcomes demonstrated that compared with TIF, administering rh-BNP markedly reduced the occurrence of SF after PCI.
In addition, the thrombus score of patients receiving treatments with rh-BNP was evidently lower than that of TIF. It may be due to the more substantial thrombolytic function of rh-BNP on existing thrombi in the CA14. Regarding biochemical parameters, the two clinically recognized myocardial function indicators, CK and CKMB, showed significantly lower peak levels in the RBG compared to the TIF group.
At the same time, side effects were absent among the sufferers participating in this experiment at the peak time point 15. In addition, the NT pro-BNP, which serves as a marker for the degree of myocardial injury, was also lower in the RBG than in the TIF group 16. These data clearly indicate that rh-BNP has a more substantial protective effect on PCI treatment-related injuries than TIF.
The electrocardiogram examination of the patient’s myocardial function revealed that the sum-STR changes in the RBG were superior to those in the TIF group. Previous studies demonstrated a positive correlation between the recovery of myocardial ischemic injury and the recovery of sum-STR 17. Integrated with the significant changes in LVEF in the RBG, it can be seen that the improvement in the influence of rh-BNP on myocardial function is also more marked than that of TIF. In addition, the incidence of MACE in the RBG was below that in the TIF group, representing rh-BNP’s safety in clinical application. This study followed all patients for 30 days after discharge, and the results showed no differences in biochemical, myocardial function, MACE, and other parameters between the two groups of patients, further proving the potential of rh-BNP in improving CA BF after PCI surgery. Existing research also indicates that the influence of rh-BNP on the heart is more pronounced after intervening, but over time, the disparity in treating efficacy in the two drugs decreases. This decrease may be because of the more substantial function of rh-BNP in enhancing microcirculation by dissolving small blood clots 14.
In conclusion, the current research compared the effectiveness of rh-BNP and TIF in preserving STEMI patients from PCI-related ischemia/reperfusion (I/R) injury. The results show that both drugs significantly reduce the occurrence of SF and MCAE and improve myocardial function. Additionally, during the 30-day follow-up, rh-BNP had a more substantial immediate effect on most indicators after the intervention than TIF. The safety of its application was similar, suggesting good potential for clinical use in treating PCI-related SF.
Notably, the study has various limitations. Firstly, it is a retrospective study using case data, potentially introducing bias and limiting the findings’ generalizability. Secondly, the sample size is relatively small. Thirdly, the study lacks information on the long-term outcomes of the two treatment methods, which is crucial for understanding their overall effectiveness and safety.












 uBio
uBio