Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Archivos Venezolanos de Farmacología y Terapéutica
versión impresa ISSN 0798-0264
AVFT v.20 n.1 Caracas feb. 2001
Archivos Venezolanos de Farmacología y Terapéutica, Volumen 20 - Número 1, 2001 (84-87)
Increased Serum Malondialdehyde and Decreased Nitric Oxide within 24 hours of Thrombotic Stroke Onset
C Cano1, V Bermúdez1, HE Atencio2, M Medina1, A Souki1, A Amell1, O Molina3, H Restrepo1, ME Vargas1, M Núñez1, A Pérez1 and M Ambard1.
- Centro de Investigaciones Endocrino - Metabólicas "Dr. Félix Gómez", Facultad de Medicina, Universidad del Zulia, Maracaibo, Venezuela.
- Servicio de Neurología, Hospital Chiquinquirá, Maracaibo, Venezuela.
- Servicio de Neurología, Hospital Universitario, Maracaibo, Venezuela.
ABSTRACT
Background and purpose: Ischaemia/reperfusion generates free oxygen radicals, that react with the unsaturated lipids of biomembranes resulting in the generation of products such as malondialdehyde (MDA). MDA could be a sensor for tissue damage and reperfusion. Nitric oxide (NO), released due to the early arrival of leukocytes to the brain parenchyma, could be a sensor for non-flow phenomenon. Thereby, the purpose of this research was to evaluate the behavior of MDA and NO within the first 24 hours after the stroke onset.
Methods: Fifteen patients aged between 49 and 87 years, admitted to the emergency of University Hospital and Chiquinquirá Hospital in Maracaibo, Venezuela, were examined by a neurologist and underwent 12-lead ECG and brain CT scan for the diagnosis of thrombotic stroke. Serum MDA and NO were measured as thiobarbituric acid adducts and total nitrites. Data were collected within the first 24 hours after the stroke onset.
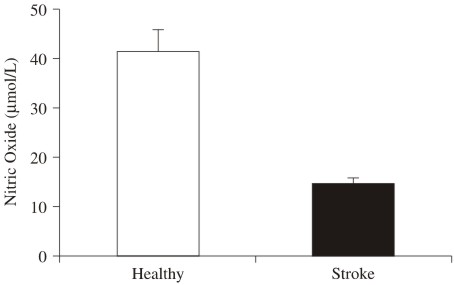
Results: MDA for patients with stroke had a significant increase (p<0.001) when compared with healthy controls (47.9 ± 7.1 vs. 1.7 ± 0.2 mmol/L). Conversely, serum NO for patients with stroke had a significant decrease (p<0.001), when compared with the group control (14.5 ± 1,4 vs. 41,3 ± 3,7 mmol/L). The lowest values of MDA and the highest values of NO were observed in two patients, who died.
Conclusions: MDA increases and NO diminishes within the first 24 hours after the thrombotic stroke onset. This suggests that the MDA could be used as a potential reliable and sensitive sensor for reperfusion, whereas NO could acts as a potential biochemical sensor for non-reflow phenomenon.
Key Words: Stroke, Nitric oxide, Malondialdehyde, Ischemia, Reperfusion.
INTRODUCTION
Brain ischaemia describes a condition that exists when fractional uptake of oxygen in the brain is not sufficient to maintain the rate of cellular oxidation, leading to metabolic changes and consequeant of cellular death. During ischaemia, enzymes and some ions like Fe+3 and Cu+2 involved in oxide-reduction pathways change to a reduced mode which, during reperfusion, become a source of electrons for free oxygen radicals formation through Fenton and Haber–Weiss reactions. Restoration of bloud flow might result in numerous further negative consequences such as free oxygen radicals superoxide (O2•–) and hydroxyl (•OH) which react with the unsaturated lipids of biomembranes, resulting in the generation of lipid peroxide radicals (ROO•), lipid hidroperoxides (ROOH) and fragmentation products, such as malondialdehyde (MDA). This suggests that MDA could be a sensor for tissue damage and reperfusion(1).
An inflammatory reaction is a common response of the brain parenchyma to various forms of insult(2). The early arrival of leukocytes in the brain parenchyma is independent from the presence of necrosis, and this idea leads to the hypothesis that these cells play a role in the progression from brain ischaemia to brain infarction(3). There are a number of mechanisms by which leukocytes may produce deleterious effects on ischaemic parenchyma. It has been proposed that leukocytes obstruct microvessels and contribute toward the non-reflow phenomenon(4). Other detrimental effects of leukocytes during ischaemia may be due to the release of vasoconstrictive mediators, such as superoxide radical, thromboxane A2, endothelin-1, prostaglandin H2, proteolitic enzymes, such aselastase, nitric oxide (NO) and lipidic hidroperoxides(5). The aim of this study was to evaluate the serum levels of MDA and NO within the first 24 hours after the stroke onset as both potential sensors of reperfusion and tissue damage, respectively.
SUBJECTS AND METHODS
The sample consisted of fifteen patients admitted to emergency of University Hospital and Chiquinquirá Hospital in Maracaibo, Venezuela; these patients were examined by a neurologist and underwent standard blood test (blood and ionograms, blood cell count, coagulation test and erythrocyte sedimentation rate), 12-lead ECG, and non-contrast computed tomography brain scan (CT). A medical history for each patient was recorded using all available resources and the following data were collected prospectively: age, gender, education level, presence of hypertension, current treatment with antihypertensive drugs, diabetes mellitus and current use of antidiabetic drugs, hyperlipidemia, history of peripheral artery disease with intermittent claudication, previous TIA or stroke; mean alcohol consumption; number of cigarettes consumed per day or cessation derning the lant 5 year-period; use of aspirin, antioxidants, and presumed cause of stroke. The level of consciousness was evaluated in each patient on admission. Data were recorded as soon as possible after onset and always within the first 24 hours.
The group control consisted of 8 men and 7 healthy women with an average age of 56.7 ± 1.3 years (range 50 to 69 years) not statistically different from stroke patients. These subjects did not have history of previous TIA or stroke, alcohol consumption, cigarette smoking, high blood pressure, coronary artery disease, diabetes mellitus or hyperlipidemia.
Statistical analysis
Data were expressed as mean ± standard error and were analyzed with a commercially available program (SPSS version 7.2 for Windows). Comparisons between patients with stroke and healthy subjects were evaluated by two-tailed unpaired student’s t-test. Differences were considered statistically significant at a value of p<0.05.
Malondialdehyde and Nitric Oxide quantification
Malondialdehyde, a breakdown product of peroxidized polyunsaturated fatty acids, serve as a convenient marker of lipid peroxidation. Thiobarbituric acids adducts of MDA generate a stable cromophore with maximal absorbance at 532 nm. Proteins, lipids and aldehydes other than MDA were eliminated prior to a colorimetric assay(6). This assay has a sensitivity of 0.1
mmol/L.Nitric oxide was measured in serum using a colorimetric assay for determination of total nitrites. NADH-dependent enzyme nitrate reductase for quantitative conversion of nitrate to nitrites was used prior to quantification of nitrite using Greiss reagent(7). This assay has a sensitivity of 1
mmol/L.
RESULTS
Out of the 15 patients admitted, 8 were men and 7 were women with an average age of 64 ± 3.6 years (range, 49 to 87 years). The fifteen patients had a thrombotic stroke (100%); 33.3% were hit in the right middle cerebral artery and 66.6% were affected in the left middle cerebral artery. Fourteen patients (93.3%) showed high blood pressure but only five patients received antihypertensive treatment, which consisted of 3 with enalapril, 1 with captopril, 1 with furosemide. None of the patients had been using aspirin or antioxidant therapy and only three of them suffered from type 2 diabetes mellitus (20%) (Table 1). From the neurological point of view, six patients had aphasia (40%) and two had dysarthria (13.3%). All patients had hemiparesis (100%); nine of them had Babinsky (60%); two patients had hemihypoesthesia (13.3%); four patients had sight paralysis (26.6%); eleven patients had normal consciousness (73.3%); one patient was in coma (6.6%); one patient had inattention (6.6%) and two patients had stupor (13.3%). Fatal stroke was present in two patients (13.3%) (Table 2).
Serum MDA was dramatically increased for stroke patients (47.9 ± 7,1 mmol/L) when compared to healthy controls (1.7 ± 0.2 mmol/L) p<0,001 (Figure 1).
Serum NO measured as total nitrites had a significant decrease (14.5 ± 1.4 mmol/L) when compared to healthy controls (41.3 ± 3.7 mmol/L) p<0,001 (Figure 2).
The two patients with fatal stroke had the lowest MDA concentrations (4.9 and 4.0 mmol/L) and the highest NO values (26 and 22 mmol/L) (Table 2).
Table 1: Clinical findings of stroke patients enrolled in the study
| P | Age | Sex | Stroke Type | S-H | Diabetes | HBP | HBP treatment |
| 1 | 49 | F | T(LMCA) | - | + | + | N/T |
| 2 | 76 | M | T(LMCA) | - | - | + | N/T |
| 3 | 87 | M | T(LMCA) | - | - | + | N/T |
| 4 | 54 | M | T(RMCA) | - | - | + | N/T |
| 5 | 54 | M | T(LMCA) | - | - | + | N/T |
| 6 | 55 | F | T(RMCA) | - | - | + | Enalapril |
| 7 | 50 | F | T(RMCA) | TIA | - | + | Enalapril |
| 8 | 83 | F | T(LMCA) | - | - | + | Captopril |
| 9 | 83 | F | T(LMCA) | - | - | + | Furosemide |
| 10 | 52 | M | T(LMCA) | - | - | + | N/T |
| 11 | 48 | M | T(RMCA) | - | - | + | N/T |
| 12 | 77 | M | T(LMCA) | - | - | - | - |
| 13 | 65 | F | T(LMCA) | TIA | + | + | Enalapril |
| 14 | 64 | F | T(RMCA) | - | - | + | N/T |
| 15 | 64 | F | T(LMCA) | - | + | + | N/T |
Abbreviations: P = Patient, F = Female, M = Male, S-H = Stroke history, HBP = High blood pressure, N/T = No treatment, T = thrombotic stroke, TIA = Transient ischaemic attack, LMCA = Left middle cerebral artery, RMCA = right middle cerebral artery.
Table 2: Neurological and oxidative findings of stroke patients enrolled in the study.
| P | A | D | H-P | C-N | B | H-H | S-P | S-C | Death | MDA ( mmol/L) | NO ( mmol/L) |
| 1 | + | + | + | + | + | - | - | NC | - | 109.1 | 11 |
| 2 | - | - | + | + | + | - | - | C | - | 43.6 | 13 |
| 3 | + | - | + | + | + | - | - | NC | - | 31.6 | 11 |
| 4 | - | - | + | + | - | + | - | NC | - | 39.6 | 15 |
| 5 | - | - | + | + | - | + | - | NC | - | 55.3 | 17 |
| 6 | - | - | + | + | + | - | - | I | - | 74.6 | 19 |
| 7 | - | + | + | + | + | - | - | NC | - | 78.3 | 16 |
| 8 | - | - | + | + | + | - | + | S | + | 4.9 | 26 |
| 9 | + | - | + | + | + | - | + | NC | - | 38.8 | 7 |
| 10 | + | - | + | + | - | - | + | NC | - | 30.0 | 21 |
| 11 | - | - | + | + | - | - | - | NC | - | 73.1 | 10 |
| 12 | + | - | + | + | - | - | + | S | + | 4.0 | 22 |
| 13 | + | - | + | + | + | - | - | NC | - | 43.6 | 9 |
| 14 | - | - | + | + | + | - | - | NC | - | 40.9 | 11 |
| 15 | - | - | + | - | - | - | - | NC | - | 51.1 | 10 |
Abbreviations: P = Patient, A = Aphasia, D = Dysarthria, H-P = Hemiparesis, C-N = Cranial nerves, B = Babinsky, H-H = Hemihypoesthesia, S-P = Sight paralysis, S-C = state of consciousness, NC= Normal consciousness, C = Coma, S = Stupor, I = Inattention, MDA = Malondialdehyde, NO = Nitric Oxide.
Figure 1: Serum MDA levels within 24 hours onset thrombotic stroke, White column represents MDA for healthy subjects and black column MDA for stroke. Note that MDA levels increased significantly after stroke onset (p< 0.001).
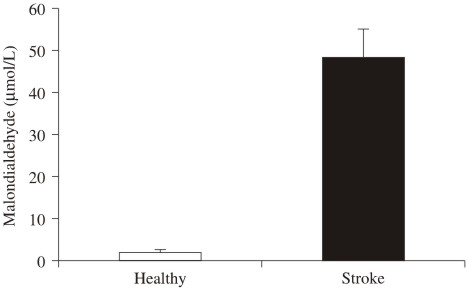
Figure 2: Serum NO levels within first 24 hours onset thrombotic stroke,white column represents NO for healthy subjects and black column NO for stroke. Note that NO levels decreased significantly after stroke onset (p< 0.001).
DISCUSSION
Our findings show a dramatic increase in serum MDA values and also a significant decrease in NO within the first 24 hours after the thrombotic stroke onset. The source of such amount of MDA is oxygen free radicals superoxide (O2•–) and hydroxile (•OH) generated during reperfusion that reacts to the unsaturated lipids of biomembranes. As it can be observed in Table 1, the two patients with fatal stroke had the lowest concentrations of MDA: 4.0 and 4.9
mmol/L. Although this study did not assess the biochemical mechanisms that might explain this finding, it could the possible that early arrival of leukocytes to the brain parenchyma obstructed the microvessels and contributed to the so-called "non-reflow" phenomenon and, thereby, the decrease in MDA production(2,4). Evidence of this, are the highest concentrations of NO (22 and 26 mmol/L) observed in the two patients who died. These findings are consistent with data, which had shown a smaller infarct volume in neutropenic animals than those observed in normal controls(8). Furthermore, a significant correlation was found in humans between the degree of leukocyte accumulation and infarct volume as assessed by CT(9). Human data demonstrated an increased number of leukocytes in the cerebral fluid of acute stroke patients 2 to 3 days after the stroke(10) and one autopsy study described intense leukocyte infiltration of the brain parenchyma 2 to 3 days after the stroke(11). Lower levels in NO within the 24 hours after the stroke onset in 87% of patients who survived, might have been a protection mechanism(12,13). This is consistent with reports that show a selective inhibition of inducible nitric oxide synthase preventing ischaemic brain injury in rats(14), and a decrease in those patients who suffered brain ischaemia. According to data published by our laboratory, during the acute phase of myocardial infarction both NO and MDA showed a dramatic increase, which may mean that MDA is a marker for ischaemia/reperfusion, but NO levels behave in heart and brain in different ways(15).We conclude that NO and MDA have a high potential to be used as reliable sensors for reperfusion and non-reflow phenomenon within the first 24 hours after the stroke onset.
REFERENCES
1. Frei B. Reactive oxygen species and antioxidants vitamins, mechanism of action. Am J Med. 1994; 97: 5-12. [ Links ]
2. Hallenbeck JM: Significance of the inflammatory response in brain ischaemia. Acta Neurochir Suppl (Wien). 1996; 66: 27-31. [ Links ]
3. Pantoni L, Sarti C, Inzitari D: Cytokines and cell adhesion molecules in cerebral ischaemia. Arterioscler Thromb Vasc Biol. 1998; 18: 503-513. [ Links ]
4. Hallenbeck JM, Dutka AJ, Tanishima T, Kochanek PM, Kumaroo KK,Thompson CB, Obrenovitch TP, Contreras TJ: Polymorphonuclear leukocyte accumulation in brain regions with low blood flow during the early postischaemic period. Stroke. 1986; 17: 246-53. [ Links ]
5. Fridovich I. The biology of oxygen radicals. Science. 1978; 201: 875-80. [ Links ]
6. Draper H, Squires E, Mah H, Wu J, Agarwal S, Hadley M. A comparative evaluation for thiobarbituric acid methods for the determination of malondialdehyde in biological materials. Free Radic Biol Med. 1993; 15: 353-363. [ Links ]
7. Archer S: Measurement of nitric oxide in biological models. FASEB J. 1993; 7: 340-360. [ Links ]
8. Chen H, Chopp M, Bodzin G: Neutropenia reduces the volume of cerebral infarct after transient middle cerebral occlusion in the rat. Neurosci Res Commun. 1992; 11: 93-99. [ Links ]
9. Akopov SE, Simonian NA, Grigorian GS: Dynamics of polymorphonuclear leukocytes accumulation in acute cerebral infarction and their correlation with brain tissue damage. Stroke. 1996; 27: 481-489. [ Links ]
10. Sörnäs R, Ostlund H, Muller R: Cerebrospinal fluid cytology after stroke. Arch Neurol. 1972; 26: 489-501. [ Links ]
11. Chuaqui R, Tapia J: Histologic assessment of the age of recent brain infarcts in man. J Neuropathol Exp Neurol. 1993; 52: 481-489. [ Links ]
12. Ladecola C, Zhang F, Casey R, Clark HB, Ross ME. Inducible nitric oxide synthase gene expression in vascular cells after transient focal cerebral ischaemia. Stroke. 1996; 27: 1373-80. [ Links ]
13. Buisson A, Plotkine M, Boulu RG: The neuroprotective effect of a nitric oxide inhibitor in a rat model of focal cerebral ischaemia. Br J Pharmacol. 1992; 106: 766-7. [ Links ]
14. Parmentier S, Böhme GA, Lerouet D, Damour D, Stutzmann JM, Margaill I, Plotkine M: Selective inhibition of inducible nitric synthase prevents ischaemic brain injury. Br J Pharmacol. 1999; 127: 546-552. [ Links ]
15. Bermúdez B, Bracho V, Bermúdez F, Medina M, Núñez M, Amell A, Cano P: Comportamiento del malondialdehído y del oxido nítrico séricos en pacientes con infarto del miocardio. Rev Esp Cardiol. 2000; 53: 502-506. [ Links ]













